Looking beyond joint counts: Exploring what happens in psoriatic arthritis by looking at blood, synovial fluid, and synovial tissue – Dr Ryan Hum speaks to Arthritis Digest
Arthritis Digest is a magazine for people with arthritis that highlights the latest relevant research and reviews topical issues.
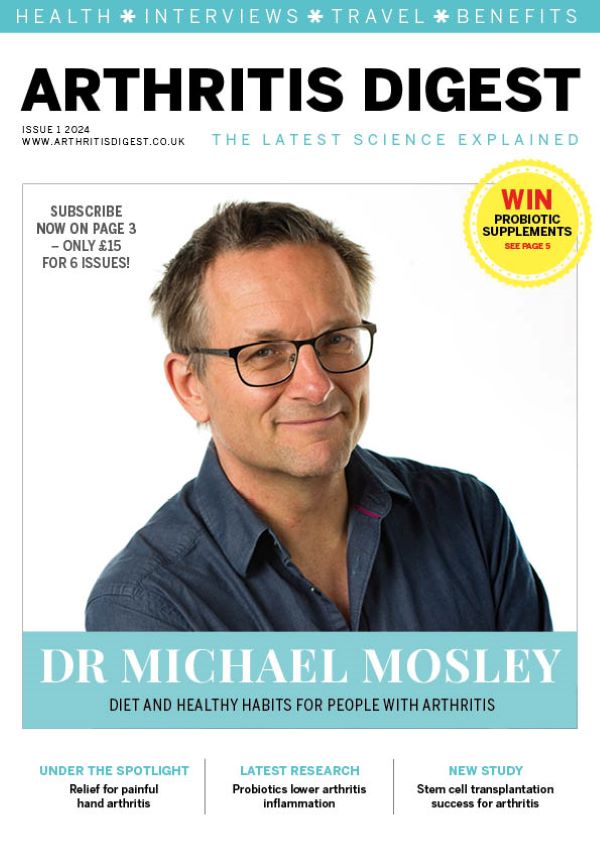
Continuing regular contributions from our Rheumatic and Musculoskeletal Diseases theme researchers, Dr Ryan Hum, Specialist Registrar in Rheumatology at Manchester University NHS Foundation Trust and Honorary Academic Clinical Fellow at The University of Manchester, discusses his research which explores what happens in the blood, synovial fluid, and synovial tissue of people with psoriatic arthritis.
Psoriatic arthritis is one of the most common types of inflammatory arthritis after rheumatoid arthritis. It can cause joint pain, swelling and stiffness and affects about 25% of people who have psoriasis. Psoriasis and psoriatic arthritis are both autoimmune conditions, caused by a fault in the immune system which makes it attack healthy parts of the body, causing inflammation.
The complex nature of psoriatic arthritis often leads to misdiagnosis, as symptoms are similar to those of other conditions. Such diagnostic challenges can impede timely intervention, contributing to poor outcomes.
To improve outcomes for people with psoriatic arthritis we need to understand the condition’s unique characteristics by using new technology to make detailed assessments of what happens in the blood, synovial fluid, and synovial tissue.

Challenges
We have more treatments than ever before for psoriatic arthritis, including tablets known as JAK inhibitors, and injections which target specific molecules that are involved in psoriatic arthritis. Yet people still experience lower quality of life and suffer from poor health, which can reduce life expectancy. This is partly because psoriatic arthritis is considered through the same lens as rheumatoid arthritis by many doctors and researchers.
Joint counts, where doctors examine the joints by feeling for swelling and squeezing the joints to see if they are tender, are great at monitoring disease in rheumatoid arthritis where hands and wrists are affected. However, we know that psoriatic arthritis more often affects large joints which are not measured in some of the standard assessments used commonly in clinic.
Psoriatic arthritis is also distinct from rheumatoid arthritis as it is associated with skin, eye, gastrointestinal, spine and tendon involvement.
To better serve our patients with psoriatic arthritis we need to understand what is going on in the blood and in the joints in psoriatic arthritis, and how this differs to rheumatoid arthritis.
Ultrasound
As joint counts can underestimate disease severity in psoriatic arthritis, we use ultrasound scanning of the joints to get an accurate idea of which joints are inflamed as part of our research studies. It takes about an hour to scan the hands, wrists, elbows, knees, ankles and toes.
Patients in our study undergo ultrasound scanning to characterise disease activity. They generously donate blood samples, fluid taken from the joints using a needle, and samples of joint tissue. Katarzyna Lachawiec (see below) is one of our inspirational study patients who still had active disease despite treatment.
Using advanced technologies, we isolate the cells and characterise how they look and behave. As we have cells from three different places, we hope to see how cells move and change from the bloodstream to the joint fluid and then eventually into the joint tissue to cause inflammation. If we can understand this process, we might be able to develop better drugs and treatments to fix or block these disease-causing pathways so that the inflammation in psoriatic arthritis becomes completely controlled (remission).
Synovial biopsies
We know from previous studies* in rheumatoid arthritis that looking at cells in the blood only gives us a snapshot of what is happening. To be able to see what happens in the joint itself we can take samples of joint fluid in clinic by inserting a small needle through the skin into the joint. Looking at the cells in the joint fluid and the blood gives us an even better picture of what is happening.
Finally, to see what is happening in the inflamed joint tissue, we can now do ultrasound-guided synovial biopsies using special biopsy needles. Prof Pauline Ho from Manchester Royal Infirmary, part of Manchester University NHS Foundation Trust, has pioneered this technique and is now a leader in performing synovial biopsies for research purposes.
Single cell technologies
New genomic technologies now allow us to look at individual cells from patients at an affordable cost. Using these state-of-the-art technologies we can identify different cell types, see what cells are doing, how they interact, develop and travel.
We are examining the blood, synovial fluid and synovial tissue from people with psoriatic arthritis and comparing this to people with rheumatoid arthritis who have active disease detected on ultrasound scanning of 66 joints. This is thanks to funding from the National Institute for Health and Care Research Manchester Biomedical Research Centre, the British Society for Rheumatology, and the British Psoriatic Arthritis Consortium.
By understanding which cells cause problems and disease we hope to be able to discover and develop better treatments, and improved ways of monitoring disease activity and remission. The outcome will be better quality of life for people with psoriatic arthritis.
Conquering psoriatic arthritis: a journey from pain to triumph
by Katarzyna Lachawiec

When I was a young and hopeful 21-year-old in 2003, the unexpected onset of psoriatic arthritis symptoms sent shockwaves through my life. Little did I know that it would take two long years for a confirmed diagnosis.
The ordeal began with a persistent discomfort in my left ankle, which gradually evolved into an excruciating pain that seriously hindered my ability to walk, much less carry out my daily activities with ease. The initial treatment I received, sulfasalazine and methotrexate, showed limited efficacy, leaving me in a state of despair as I grappled with the relentless progression of this debilitating condition.
Months passed and the insidious grip of psoriatic arthritis tightened around more of my joints, transforming the simple act of dressing into a Herculean task. I could no longer manage basic functions independently, and the world around me seemed to be closing in. I will never forget the tears in my dad’s eyes, seeing how much I was suffering. It broke my heart.
Hospitalisation
Desperation pushed me to the edge, and the culmination of my suffering peaked when I was forced to spend an agonizing six weeks in hospital, desperately seeking respite from the relentless pain that had become my constant companion.
Hospitalisation marked a turning point. The treatment administered during those gruelling weeks proved to be a beacon of hope, gradually lessening the intensity of my pain. While it didn’t provide immediate and complete relief, it offered a glimmer of progress. With each passing day, the pain subsided slightly, and I could once again imagine the possibility of regaining control over my life.
The initial approach to managing my condition involved a combination of steroids and methotrexate, which, for a time, provided respite. However, as I inched closer to a dose of 25 milligrams injection, my body began to reject this treatment, thrusting me into a state of anxiety and uncertainty.
It was 2009, and I found myself faced with a life-altering decision – should I put my faith in a relatively new form of treatment, a biological medication called Humira? I grappled with the fear that this new medication might not work or, even worse, lose its effectiveness prematurely. The prospect of returning to the agonising pain of earlier years and the dependence on others for my daily tasks weighed heavily on my mind.
Game changer
Despite my reservations, I took the leap of faith and began treatment with Humira. The relief I experienced was nothing short of miraculous. Slowly but steadily, I began to regain a sense of normalcy. I was able to perform tasks that had once been unattainable, and the spectre of unrelenting pain receded into the background.
Reflections
Living under the oppressive shadow of long-term chronic pain is a uniquely harrowing experience. The torment gnaws away at one’s happiness, replacing it with a constant, relentless worry. The anguish saps your hope and drains your willingness to continue the battle. The world takes on a different hue when every step is a struggle, and even the simplest tasks become daunting trials.
Fourteen years later I find myself reflecting on this remarkable journey. Over the years, I’ve faced my share of trials, enduring three to four relapses that necessitated adjustments to my medication. While it hasn’t always been smooth sailing, I am deeply grateful for the advancements in medical science and the continued support of my healthcare team. Today, my life is a testament to the power of perseverance and modern medicine.
Psoriatic arthritis no longer looms as a shadow over my life; instead, I embrace the present with gratitude and optimism, celebrating the beauty of ordinary moments that were once a distant dream.

The future
Remarkable strides have been made in the medical field. The introduction of biological medications provides a lifeline to people like me, offering the prospect of a life unburdened by the tyranny of chronic pain.
In a commitment to contributing to the ongoing battle against psoriatic arthritis, I have joined Dr Ryan Hum and Prof Pauline Ho’s research programme. The programme aims to shed light on the complexities of this illness, to understand it more deeply and to explore new avenues of treatment.
I hope that one day, through the collective efforts of researchers, medical professionals, and individuals like myself, we may unlock the door to a cure for psoriatic arthritis, ensuring that no one else has to endure the pain and suffering that marked my early years with this condition.
*Zhang, Fan et al. Defining inflammatory cell states in rheumatoid arthritis joint synovial tissues by integrating single-cell transcriptomics and mass cytometry.
Floudas, Achilleas et al. Distinct stromal and immune cell interactions shape the pathogenesis of rheumatoid and psoriatic arthritis.
Penkava, Frank et al. Single-cell sequencing reveals clonal expansions of pro-inflammatory synovial CD8 T cells expressing tissue-homing receptors in psoriatic arthritis.